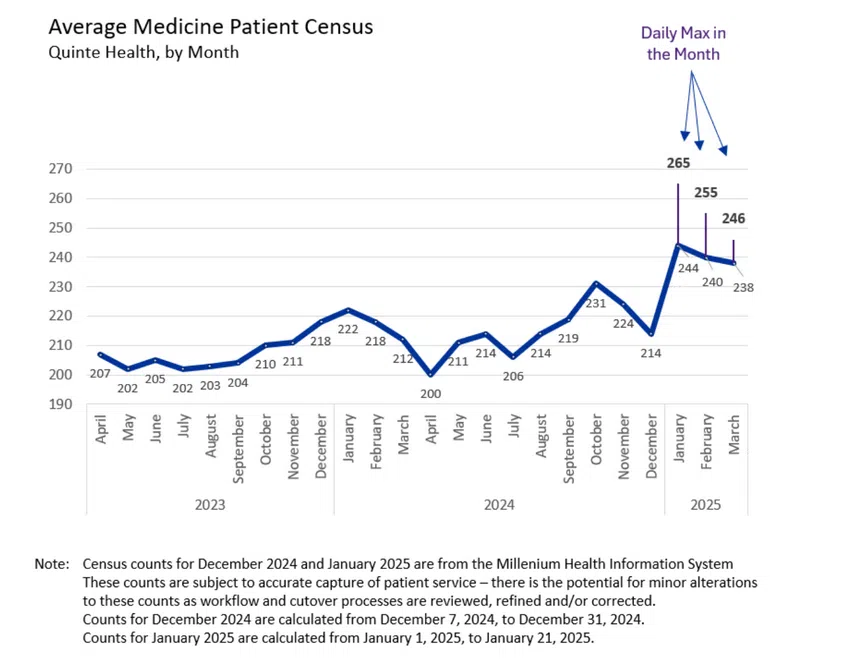
An active respiratory illness season helped to bring a record number of patients to Quinte Health hospitals over the last few months.
In her report to the board of directors at Quinte Health, President and CEO Stacey Daub says that although patient volumes have decreased from the peaks seen in January, they remain high in comparison to previous years.
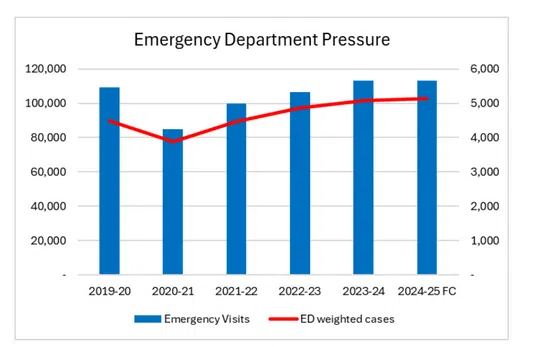
It also noted that emergency department volumes have now surpassed levels seen before 2020 due to increasing patient complexity and acuity.
Daub was asked what made this flu season notable.
“It just happened to be a very active flu season. I think it’s also true generally that vaccinations are down generally across populations, not only in Canada, but internationally. So that has an impact on the numbers and the length of an infectious disease season,” Daub tells media.
“So this year was long and hard is how I would describe it.”
When asked about more public engagement to encourage more people to be up to date with their vaccinations, Daub says there is both an individual responsibility and community responsibility to protect others.
“I’m hopeful over time that people will be able to have good information, and I think our local public health plays a big role in that to make sure that people have accurate information that they trust and that is credible and can guide them to make good decisions,” Daub said.
Despite the increase on hospital demands, Quinte Health noted that it is seeing significant progress in staffing.
Daub’s report notes that the vacancy rate has been reduced from 12% in 2023 to 6.3% in 2025.
There have been 437 new team members hired in 10 months at the organization, including 271 student recruits.
The majority of those student recruits are from Loyalist College.
It was also noted that before the increase in patient volumes during the winter months, work had been done to improve wait times in the Emergency Department at Quinte Health hospitals.
Committee Chair Nancy Evans outlined in her report that that was a priority for 2024.
She says a taskforce composed of physicians, nurses, and staff spearheaded the changes.
Those changes included the introduction of the Go Zone, a model designed to improve efficiency by restructuring how patients are triaged and
treated.
By replacing the previous Green and Yellow Zones with a new ambulatory and non-ambulatory care model, Evans says the ED was able to optimize the use of available space and resources.
This change lead to a 27% reduction in the number of patients leaving without being seen, dropping from 9.6% in September to 7.0% in November.
Time from triage to in-room assessment improved by 13%, decreasing from 4.5 hours to 3.9 hours, while the physician initial assessment time was reduced by 16%, from 7.2 hours to 6.1 hours.
The overall length of stay for non-admitted patients saw a 16% reduction, improving from 10.2 hours in September to 8.6 hours in November.






